Endometriosis
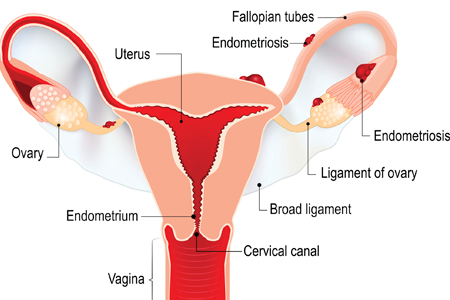
A condition that typically occurs during a woman's childbearing years, endometriosis happens when the tissue growing inside the uterus — endometrial tissue — also grows outside the uterus into the pelvis and abdomen. In rare cases, endometrial tissue can spread and grow in other areas of your body.
Each month, the endometrial tissue inside your uterus thickens. After ovulation, if you don't become pregnant, the endometrial tissue sheds and bleeds in a process known as menstruation. With endometriosis tissue, the same thing happens, causing pain and inflammation in the areas with endometriosis outside the uterus. Surrounding tissue becomes irritated. Scar tissue and adhesions result, causing pelvic tissues and organs to essentially stick together. When this happens inside the ovaries, blood-filled cysts called endometriomas can form. Over time, this monthly process causes pain that can be severe, and fertility problems may develop.
Who gets endometriosis?
If you're a menstruating female, you can have endometriosis. You can develop it as young as your teen-age years, and it may continue until you go through menopause.
There does seem to be a genetic connection. It's not uncommon to see mothers, daughters and sisters who have endometriosis.
Patients with certain uterine anomalies (abnormalities) can develop endometriosis over time due to a blockage of the menstrual flow and the shedding of endometrial tissue. This material drains through the fallopian tubes back into the pelvis, allowing endometrial cells to implant in the pelvic organs outside the uterus.
What causes endometriosis?
There are different theories about how endometriosis develops:
- Retrograde menstruation, when endometrial cells and menstrual blood back up through the fallopian tubes, is the most popular theory
- Endometrial cells travel through blood vessels into other organs and spread that way
- Some cells of the tissue normally surrounding the organs transform themselves into endometriosis cells
It's known that estrogen feeds endometriosis cells. Because estrogen levels drop at menopause, symptoms typically subside.
What are endometriosis symptoms?
- Pain: You might feel pain in your lower abdomen, rectum, vagina or lower back, depending on where the endometrial tissue is growing. Pain is typically worse in the week leading up to your period until your period has subsided. You also may have pain during sex, when you have a bowel movement or when you urinate. Over time, this pain can become constant.
- Excessive bleeding: You may have heavy bleeding during periods and/or bleeding between periods.
- Infertility: You may have issues getting pregnant. This may happen whether or not you also experience pain.
The severity of the pain doesn't always correlate with the severity of the condition. You can have mild endometriosis with severe pain and advanced endometriosis (and resulting infertility issues) with virtually no pain.
How is endometriosis diagnosed?
Endometriosis is suspected based on your symptoms, and family history may make it more likely. Your HonorHealth gynecologist may do a pelvic exam and/or pelvic ultrasound, and may then prescribe medication to see if your symptoms improve.
The only way to definitively diagnose endometriosis is by laparoscopic surgery.
In rare cases, endometriosis-like symptoms may also be caused by abnormalities of the uterus, such as adenomyosis and uterine fibroids.
How is endometriosis treated?
There's no cure for endometriosis, but treatment can help. It depends on whether you're treating pain, infertility or both.
For pain, treatment options include:
- Over-the-counter pain medicines such as ibuprofen or naproxen
- Hormonal manipulation using birth control pills, patches, vaginal rings, progesterone-only formulations, and medications like Lupron that cause a transitory menopause
- Hormone therapy, including progestin therapy or gonadotropin-releasing hormone (Gn-RH) agonists and antagonists
- Minimally invasive endometriosis surgery to:
- Remove small endometriosis implants, nodules, adhesions and cysts from the ovaries
- Open blocked, nonfunctional fallopian tubes
- Hysterectomy (removing the uterus), which probably also will involve removing the ovaries to shut down hormonal activity feeding the endometriosis cells
Your treatment choice may depend on whether you want to get pregnant, treatments you've had previously, and how close you are to menopause.
If you're experiencing infertility as a result of endometriosis, you and your HonorHealth gynecologist will likely discuss minimally invasive surgery followed by infertility treatment to help you conceive as soon as possible after you've healed from surgery.