Cerebrovascular disorders
Arteriovenous malformation and dural arteriovenous fistula are cerebrovascular disorders diagnosed and treated at HonorHealth hospitals.
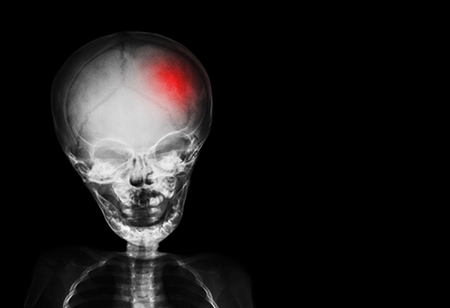
Arteriovenous malformation
A cerebral arteriovenous malformation is an abnormal connection that usually forms before birth between arteries and veins in the brain. The cause is unknown. The condition occurs when arteries in the brain connect directly to nearby veins without having the normal vessels (capillaries) between them.
Arteriovenous malformations vary in size and location in the brain. A rupture occurs because of pressure and damage to brain tissue, as well as a lack of blood flow to the brain. Symptoms also can occur when large arteriovenous malformations that have not bled press on the brain tissue.
Arteriovenous malformation occurs in less than 1% of people. Although the condition is present at birth, symptoms can occur at any age. Hemorrhages occur most often in individuals between the ages of 15 to 20 but also can occur later in life. Some patients with an arteriovenous malformation also have cerebral aneurysms.
There often are no symptoms until the arteriovenous malformation ruptures. This results in sudden bleeding in the brain (hemorrhagic stroke). In more than half of patients with arteriovenous malformation, hemorrhage is the first symptom. Symptoms of arteriovenous malformation hemorrhage are the same as those of other intracerebral hemorrhages.
Diagnosis of an arteriovenous malformation
Physical and neurological exams are needed, but they could be completely normal. Your HonorHealth neurologist might use some of these tests to diagnose an arteriovenous malformation:
- Cerebral angiogram
- Cranial MRI
- Electroencephalogram (EEG)
- Head CT scan
- Magnetic resonance angiography (MRA)
Treatment options for arteriovenous malformation
A bleeding arteriovenous malformation is a medical emergency. The treatment goal is to prevent further complications by controlling the bleeding and seizures and, if possible, removing the arteriovenous malformation.
Treatments (some are used together) include:
- Open brain surgery
- Endovascular treatment
- Radiosurgery
- Open brain surgery removes the malformation through an opening made in the skull
- Embolization (endovascular treatment): The injection of a glue-like substance into the abnormal vessels to stop blood flow in the arteriovenous malformation and reduce the risk of bleeding. This may be the first choice for some kinds of arteriovenous malformations or if surgery cannot be done.
- Stereotactic radiosurgery. This procedure delivers radiation directly to the area of the arteriovenous malformation to cause scarring and shrinkage. The procedure can control bleeding and other symptoms and is particularly useful for small, deep arteriovenous malformations that are difficult to remove by surgery.
Dural arteriovenous fistulas
A dural arteriovenous fistula is a site of abnormal connectivity between arteries and veins, where the abnormal connection, or fistula, lies in the covering of the brain or spinal cord known as the dura.
Unlike arteriovenous malformations, which are thought to be present from birth, cranial dural arteriovenous fistulas often develop later in life after blockage or thrombosis of a cranial dural venous sinus. When a venous sinus blocks off, the brain can try to compensate by moving venous blood across other collateral pathways. In this process, however, a fistula might form, representing an abnormal collateral pathway to drain blood away from the brain. This could occur due to chronic central nervous system infection, brain trauma or a patient with a tendency to experience thrombosis.
Dural arteriovenous fistula can occur:
- In the brain: A cranial dural arteriovenous fistula is supplied by branches of the carotid artery and possibly also by branches of the vertebral artery before these arteries penetrate the dura. The fistula usually resides in the dura overlying the brain hemisphere or in the dura between the forebrain and hindbrain.
- In the spine: A spinal dural arteriovenous fistula is supplied by dural arterial branches arising from the aorta's spinal arteries. The fistula itself is in the spinal nerve root dural sleeve. Typically, a spinal dural arteriovenous fistula occurs somewhere in the lower half of the spine.
Cranial dural arteriovenous fistula is more commonly diagnosed in women over 40, while spinal dural arteriovenous fistula is more commonly diagnosed in men over 40.
Depending on the location of the fistula, symptoms of dural arteriovenous fistula in the head may be a whooshing sound heard by the patient, or abnormal eye bulging and pulsation, and impairment of vision and/or eye movement. Isolated but persistent headaches or symptoms of a brain hemorrhage, including a sudden severe headache, neurological impairment and/or collapse, are also common.
Symptoms of a spinal dural arteriovenous fistula may be slow but progressive loss of function in the limbs (more often the legs than the arms), bowel and bladder dysfunction including incontinence, and progressive erectile dysfunction in males.
Diagnosis of dural arteriovenous fistula
Any of the above symptoms and signs may lead to investigation by your specialist. Unfortunately, in the case of spinal dural arteriovenous fistula, the diagnosis may be missed or delayed because such lesions occur so rarely, and when they do occur, their symptoms and signs may be mistaken for disk disease or spinal cord inflammation.
For a cranial dural arteriovenous fistula, regular CT scanning is not very helpful in diagnosing a fistula, but it might show a hemorrhage from a fistula. CT angiography, which is CT arteriography plus CT venography, is helpful in defining a cranial fistula; so are MRI techniques. However, the standard for the detection and characterization of a dural arteriovenous fistula is cerebral angiography.
For a spinal dural arteriovenous fistula, the standard is selective spinal angiography. In this process, a catheter is used to inject multiple spinal segmental arteries arising from the aorta, one by one, until the fistula is found and characterized.
Treatment options for dural arteriovenous fistula
The two main ways of treating a dural arteriovenous fistula are through:
- Open surgery: The goal of surgery is to physically disconnect the fistula in the dura, with particular attention to obliterating the draining vein. Open surgery for a dural arteriovenous fistula typically has a very high success rate.
- Endovascular surgery: This involves a catheter-based technique of squirting "glue" into the arteries feeding the dural arteriovenous fistula or directly into the vein draining the fistula. This process is known as embolization. Sometimes, embolization is used alone to obliterate the fistula, or it may be used as an additional option prior to open surgery to help shut down as much of the fistula as possible.